PRESS RELEASE
Date: 30 June 2021
Date: 30 June 2021
Leprosy charity provides emergency COVID-19 relief to those most in need
Charity fears programmes disruption and increased leprosy disability due to pandemic
Charity fears programmes disruption and increased leprosy disability due to pandemic
The signs that COVID-19 is being defeated in the UK are encouraging, but the same cannot be said for some other parts of the world.
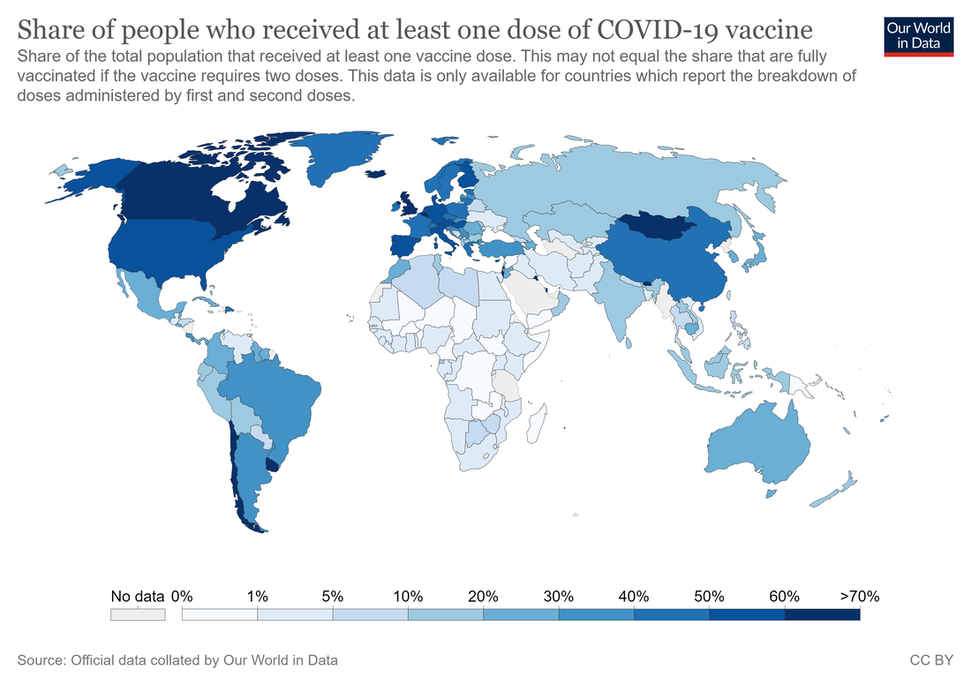
Recently published figures in Our World in Data show that the 23 countries which are endemic for leprosy* have the lowest rates of COVID-19 vaccination in the world. The World Health Organization has identified the 23 global priority countries for leprosy, where 95.9% of people detected with leprosy are found.
Recently published figures in Our World in Data show that the 23 countries which are endemic for leprosy* have the lowest rates of COVID-19 vaccination in the world. The World Health Organization has identified the 23 global priority countries for leprosy, where 95.9% of people detected with leprosy are found.
The UK Times correspondent in Delhi, recently reported that India is trying to vaccine its 1.3 billion people, but a survey has shown that 63 per cent of rural Indians and 40 per cent in small towns have no idea how to register for a vaccine. For those living with leprosy in remote communities, the situation is far worse.
“In our 125-year history, I don’t think we’ve known more challenging times” said SFLG Chief Executive Officer, Clare McIntosh. “People affected by leprosy are the most marginalised and impoverished group in the world. They often live in remote and isolated locations and have no means to travel to a clinic.”
“My heart breaks at the thought of what is happening to this vulnerable group of people who need our support now, more than any other time in SFLG’s history. And I am increasingly concerned that many leprosy programmes will have fallen behind or ceased entirely during the pandemic, especially active case-finding.”
“Our TRACE operating strategy focuses on active case-finding,” said Ms McIntosh. “In addition to providing training, research, care and emergency relief, we need to find people with leprosy if we are to treat it and stop its transmission.”
“We are also hearing that the costs of bandages, food and medication are going up, while income is getting less. But I am delighted to say that our Trustees have agreed an amazing £60,000 worth of grants across all our centres. These funds should help our centres support people with leprosy during the pandemic.”
“You only have to read a letter from one of our projects, for example, from Father Livio Prete, the Director at Dhanjuri Leprosy Centre in Bangladesh, to know how dire the situation is for people with leprosy and how grateful we are to our donors for their support right now.”
Data from a report that has just been published in the Royal Society of Tropical Medicine and Hygiene entitled “An assessment of the reported impact of the COVID-19 pandemic on leprosy services using an online survey of practitioners in leprosy referral centres” show that active-case finding projects have been reduced by 77% and an increased burden of leprosy disability in future years is predicted as a result.
For more information or interview opportunities please contact:
Clare McIntosh
Chief Executive Officer
St Francis Leprosy Guild
London W10 6EJ
Tel: +44 (0)7754 592240
Email: [email protected]
Twitter @StLeprosy
Facebook
Clare McIntosh
Chief Executive Officer
St Francis Leprosy Guild
London W10 6EJ
Tel: +44 (0)7754 592240
Email: [email protected]
Twitter @StLeprosy
About St Francis Leprosy Guild (SFLG)
SFLG is a UK-based, Catholic charity that is working towards a -leprosy-free world. We support the work of over 40 leprosy centres, clinics, hospitals, care homes and leprosy-related projects. We work in 14 countries worldwide in Africa, Asia and South America where leprosy is endemic.
About leprosy
1. What is leprosy?
Leprosy (also known as Hansen’s disease) is a complex, chronic neglected tropical disease caused by the Mycobacterium leprae bacterium. It affects the skin, the upper respiratory tract and peripheral nerves in the hands and feet, and the eyes. Leprosy can affect anyone, at any age, but it is linked to poverty, malnutrition, and genetic susceptibility.
Leprosy remains an important health problem in low and middle-income countries worldwide.
2. How is leprosy transmitted?
It is thought that leprosy is transmitted via droplets from the nose combined with prolonged, close contact with infected individuals.
3. How is leprosy diagnosed?
Leprosy is difficult to diagnose at its early stages, but it often presents as numb patches on the skin. Currently, the most reliable method to diagnose leprosy, is a slit-skin-smear test in the laboratory.
Leprosy may incubate for up to twenty years before presenting with any signs. If leprosy remains undiagnosed like this, the person affected may unwillingly transmit the disease throughout a community. However, within a short period of receiving multidrug therapy, a person affected by leprosy will no longer be infectious. If leprosy is diagnosed in its early stages, it can be treated readily, and it will not cause disabilities. Preventing disabilities from developing means people with leprosy are less likely to suffer from the stigma and discrimination that can destroy their livelihoods and entire lives.
4. How infectious is leprosy?
95% of most populations have a natural immunity to leprosy. The remaining 5% become vulnerable, mainly through poor nutrition, poor living conditions, lack of hygiene and a weakened immune system. Leprosy is not hereditary.
5. Why are people with leprosy often so disfigured?
People with leprosy lose all feeling in the affected areas and as a result, there is diminished awareness of harm from trauma or heat. Without treatment, the lack of sensation can lead to permanent damage to skin, nerves, limbs, and eyes. It can also lead to the development of reoccurring, lifelong, hard-to- treat ulcers.
6. Is there a cure? How is leprosy treated?
Leprosy can be cured using multidrug therapy (MDT), available at no cost to patients from the World Health Organization. If MDT is taken in the early stages of the disease, permanent damage to nerves is completely avoided.
7. How many are affected by leprosy in the world today?
The latest *WHO statistics reveal that in 2019 there were 202,185 new cases of leprosy diagnosed. Of concern and indicating ongoing transmission, the number of children newly detected was nearly 15,000.
These statistics do not account for those people who have leprosy with no symptoms or, who are not diagnosed and are unwittingly transmitting it to their communities. In addition, the statistics do not include those individuals who have been treated for leprosy, but whose disabilities, caused by leprosy need ongoing healthcare needs, or those who are subject to leprosy stigma and discrimination.
8. Which countries have leprosy, where is leprosy endemic?
*The WHO has identified 23 global priority countries for leprosy, where 95.9% of the global total of people detected with leprosy are found. The 23 countries are: Angola, Bangladesh, Brazil, Comoros, Cote Ivoire, DR Congo, Egypt, Ethiopia, India, Indonesia, Kiribati, Madagascar, Micronesia, Mozambique, Myanmar, Nepal, Nigeria, Philippines, South Sudan, Sri Lanka, Sudan, Somalia and Tanzania.
The highest number of people newly detected with leprosy in 2019 live in India with 114,451, followed by Brazil with 27,863 and Indonesia with 17,439.
*WHO Weekly epidemiological record, Global Leprosy Update 4 September 2020, 36, 2020, 95, 417-440
SFLG is a UK-based, Catholic charity that is working towards a -leprosy-free world. We support the work of over 40 leprosy centres, clinics, hospitals, care homes and leprosy-related projects. We work in 14 countries worldwide in Africa, Asia and South America where leprosy is endemic.
About leprosy
1. What is leprosy?
Leprosy (also known as Hansen’s disease) is a complex, chronic neglected tropical disease caused by the Mycobacterium leprae bacterium. It affects the skin, the upper respiratory tract and peripheral nerves in the hands and feet, and the eyes. Leprosy can affect anyone, at any age, but it is linked to poverty, malnutrition, and genetic susceptibility.
Leprosy remains an important health problem in low and middle-income countries worldwide.
2. How is leprosy transmitted?
It is thought that leprosy is transmitted via droplets from the nose combined with prolonged, close contact with infected individuals.
3. How is leprosy diagnosed?
Leprosy is difficult to diagnose at its early stages, but it often presents as numb patches on the skin. Currently, the most reliable method to diagnose leprosy, is a slit-skin-smear test in the laboratory.
Leprosy may incubate for up to twenty years before presenting with any signs. If leprosy remains undiagnosed like this, the person affected may unwillingly transmit the disease throughout a community. However, within a short period of receiving multidrug therapy, a person affected by leprosy will no longer be infectious. If leprosy is diagnosed in its early stages, it can be treated readily, and it will not cause disabilities. Preventing disabilities from developing means people with leprosy are less likely to suffer from the stigma and discrimination that can destroy their livelihoods and entire lives.
4. How infectious is leprosy?
95% of most populations have a natural immunity to leprosy. The remaining 5% become vulnerable, mainly through poor nutrition, poor living conditions, lack of hygiene and a weakened immune system. Leprosy is not hereditary.
5. Why are people with leprosy often so disfigured?
People with leprosy lose all feeling in the affected areas and as a result, there is diminished awareness of harm from trauma or heat. Without treatment, the lack of sensation can lead to permanent damage to skin, nerves, limbs, and eyes. It can also lead to the development of reoccurring, lifelong, hard-to- treat ulcers.
6. Is there a cure? How is leprosy treated?
Leprosy can be cured using multidrug therapy (MDT), available at no cost to patients from the World Health Organization. If MDT is taken in the early stages of the disease, permanent damage to nerves is completely avoided.
7. How many are affected by leprosy in the world today?
The latest *WHO statistics reveal that in 2019 there were 202,185 new cases of leprosy diagnosed. Of concern and indicating ongoing transmission, the number of children newly detected was nearly 15,000.
These statistics do not account for those people who have leprosy with no symptoms or, who are not diagnosed and are unwittingly transmitting it to their communities. In addition, the statistics do not include those individuals who have been treated for leprosy, but whose disabilities, caused by leprosy need ongoing healthcare needs, or those who are subject to leprosy stigma and discrimination.
8. Which countries have leprosy, where is leprosy endemic?
*The WHO has identified 23 global priority countries for leprosy, where 95.9% of the global total of people detected with leprosy are found. The 23 countries are: Angola, Bangladesh, Brazil, Comoros, Cote Ivoire, DR Congo, Egypt, Ethiopia, India, Indonesia, Kiribati, Madagascar, Micronesia, Mozambique, Myanmar, Nepal, Nigeria, Philippines, South Sudan, Sri Lanka, Sudan, Somalia and Tanzania.
The highest number of people newly detected with leprosy in 2019 live in India with 114,451, followed by Brazil with 27,863 and Indonesia with 17,439.
*WHO Weekly epidemiological record, Global Leprosy Update 4 September 2020, 36, 2020, 95, 417-440